PROVIDER SOLUTIONS
Value Care Documentation Services Vs Volume Care Payments: Medicare and payer payments to providers are driven by the value providers add to the delivered care to patients and not by the volume of patients they encounter.
Clinical Documentation Improvement (CDI) Services: Clinical notes/charts made by providers drive the medical coding process. Our highly trained staff review the documentation to substantiate the medical necessity for procedures to seek legitimate payment. This review enhances reimbursement from the payers as well as avoids recoupments, penalties, and sanctions by Recovery Audit Contractor (RAC)/ Zone Program Integrity Contractor (ZPIC).
We supply the following services to help providers remain compliant: Star ratings and quality data submission mandates such as: Physician Quality Reporting System (PQRS), Meaningful use (MU) - Electronic Health Records (EHR) Stage-II, Value Based Modifier, and Medicare Access and CHIP Reauthorization Act (MACRA) - Merit-Based Incentive Payment System (MIPS). These offerings are the new mantras for providers to remain compliant in the industry. We help providers navigate these crucial areas to assure compliance and timely payment.
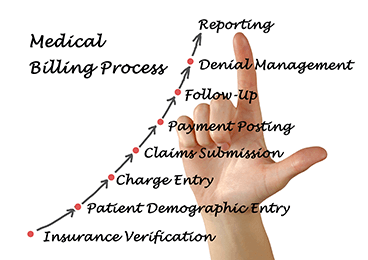
End-To-End Revenue Cycle Management Services: For traditional providers and hospitals we manage medical billing, coding, accounts receivable follow-up, and prepayment/post-payment audit compliance. Augustus HCS’ services ranges from demographic entry (CMS-1500/UB-04), charge capture, Electronic Clearing Service (ECS), Explanation Of Benefits (EOB) posting, accounts receivable follow-up and compliance assistance.